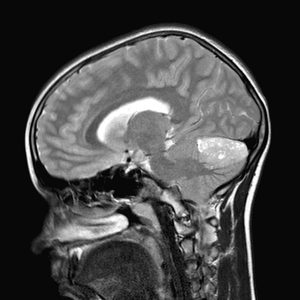
These are one of the most frequent tumours in young children. They constitute 15-20% of all tumours in children. The greatest incidence is between 8 and 9 years of age.
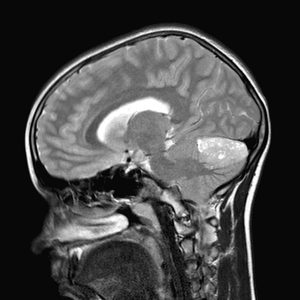 It is a fast growing tumour and so the clinical record is very short, weeks or a few months and onset is usually with intracranial hypertension due to secondary hydrocephalus and so these patients present headache, vomiting and papilloedema.
It is a fast growing tumour and so the clinical record is very short, weeks or a few months and onset is usually with intracranial hypertension due to secondary hydrocephalus and so these patients present headache, vomiting and papilloedema.
Diagnosis is based on CT scan and MRI. The treatment of medulloblastomas is always surgical. Surgery of the tumour has a double interest. First, to obtain a tissue for diagnosis of the lesion and, secondly, to remove it. On many occasions it may require placement of external ventricular drainage or a ventriculo-peritoneal shunt to treat the associated hydrocephalus. This other surgery may be required urgently at the time of diagnosis, just before surgery on the posterior fossa, or in the postoperative period. Given the complexity of this pathology, after surgery patients will be transferred to an intensive care unit for better surveillance and management.
The location of the lesion as well as the size will be factors to be taken into account when planning the surgery. In many cases intraoperative neurophysiological monitoring will be required to locate brain nuclei so as not to damage them during resection of the tumour.
The result of the analysis of the excised tumour may take between 7 and 15 days. Once the anatomy of the lesion is confirmed, consideration should be given to the administration of complementary treatment, radiotherapy or chemotherapy. Age is a determining factor for assessing radiotherapy, as it is highly damaging to brain tissue in very young children. The prongnosis will depend on the size of the tumour, the affectation of nearby structures, the dissemination or not of the tumour and the child’s age.



 It is a fast growing tumour and so the clinical record is very short, weeks or a few months and onset is usually with intracranial hypertension due to secondary hydrocephalus and so these patients present headache, vomiting and papilloedema.
It is a fast growing tumour and so the clinical record is very short, weeks or a few months and onset is usually with intracranial hypertension due to secondary hydrocephalus and so these patients present headache, vomiting and papilloedema.
